Helpers on the wrong path: Lymphocytes can force lung cancer
Th9/Th17 T helper cells stimulate the formation of metastases in lung tumors
Developing of lung cancer metastasis significantly worsens the patient’s chances for a recovery. Whether and to what extent metastases form, depends among other facts on complex regulation in the cellular environment of the primary tumor. This is significantly affected by the immune system. Scientists from the Max Planck Institute for Heart and Lung Research in Bad Nauheim and the universities in Gießen and Marburg have now been able to show that a group of lymphocytes, Th9 / Th17 cells, play an important role in this mechanism: They re-program primary tumor cells in a way that these form starting cells for metastases. The findings of the study could help to develop new targeted therapeutic approaches for the treatment of lung cancer.
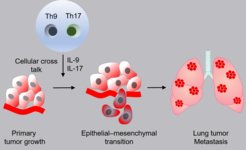
Immune cells support the development of lung metastases: The schematic diagram shows how T cells (Th9 / Th17) change lung tumor cells by releasing messenger substances. Tumor cells thereby convert into metastases.
Of all types of tumors, lung cancer is responsible for most deaths worldwide. Among other things, this may be due to the fact that it is usually not recognized before metastases have already formed. Healing thereby becomes considerably more difficult. For this reason, with a view to effective therapy, it is important to understand the processes that lead to the development of metastases.
Metastases originate in primary tumor cells that change their cell fate. Initially having the character of epithelial cells, these particular tumor cells transform in a process called epithelial-mesenchymal transition and become mesenchymal cells. This creates extremely mobile cells, which circulate through the bloodstream and subsequently form metastases elsewhere. Scientists from the Max Planck Institute for Heart and Lung Research in Bad Nauheim, together with colleagues from the Justus Liebig University in Gießen and the Philipps University in Marburg, have now been able to show that immune cells play an essential role in this epithelial-mesenchymal transition .
“One can assume that the immune system prevents the development of tumors in many cases. Immune cells normally detect and eliminate degenerated cells. However, we have now found a subpopulation of T cells that infiltrate the primary tumor and then do exactly the opposite”, says Rajkumar Savai from the Max Planck Institute, project manager in Werner Seeger's Department for Lung Development and Remodeling.
The researchers received a first clue from experiments in cell cultures. They found that activated lymphocytes in particular stimulated lung tumor cells to convert into the mesenchymal cell type. In addition, they stimulated the tumor cells to divide and migrate. "It was also striking that we were able to detect elevated levels of certain messenger substances, the cytokines IL-9 and IL-17, in the cultures," said Savai.
The scientists then looked in tissue samples from patients with a small-cell lung tumor to confirm the finding. With the help of a computer-based imaging method, it was possible to create a spatial reconstruction of different cell types and marker proteins within the tissue samples. "This allowed us to see infiltrated T-helper cells in the area between tumor cells, called stroma, including the Th9 and Th17 subpopulations," explains Friedrich Grimminger, director at the Medical Clinic at the University of Gießen. It was particularly striking that the survival rate was significantly lower in the group of patients with an above-average proportion of Th9 / Th17 cells.
In animal studies in mice, the Max Planck researchers finally demonstrated that the Th9 / Th17 cells were responsible for both the epithelial-mesenchymal transition and the subsequent migration activity of the converted cells. In addition, mice injected with Th9 / Th17 cells in addition to tumor cells developed significantly more metastases than animals that had not received lymphocytes. “When we carried out an experiment with mice that were given neutralizing antibodies against Il-9 and Il-17, we found that the effects of the Th9/ Th17 cells proceed via these two messenger substances: As a result of the antibody treatment, significantly fewer metastases formed in treated mice than in control animals,” said Savai.
With regard to a later clinical application, this experiment is particularly important. "We will next investigate whether antibody treatment against IL-9 and Il-17 could represent a new immune-based therapy concept for lung tumors," says Werner Seeger, director of the lung development and remodeling department at the Max Planck Institute . We also will investigate whether and how the complex system of different immune cells and messenger substances can be influenced in such a way that a therapy finally succeeds.
MH
